Multiparameter patient monitor (classification of monitors) can provide first-hand clinical information and a variety of vital signs parameters for monitoring patients and rescuing patients. According to the use of monitors in hospitals, we have learned that each clinical department cannot use the monitor for special use. In particular, the new operator does not know much about the monitor, resulting in many problems in the use of the monitor, and can not fully play the function of the instrument. Yonker shares the usage and working principle of multiparameter monitor for everyone.
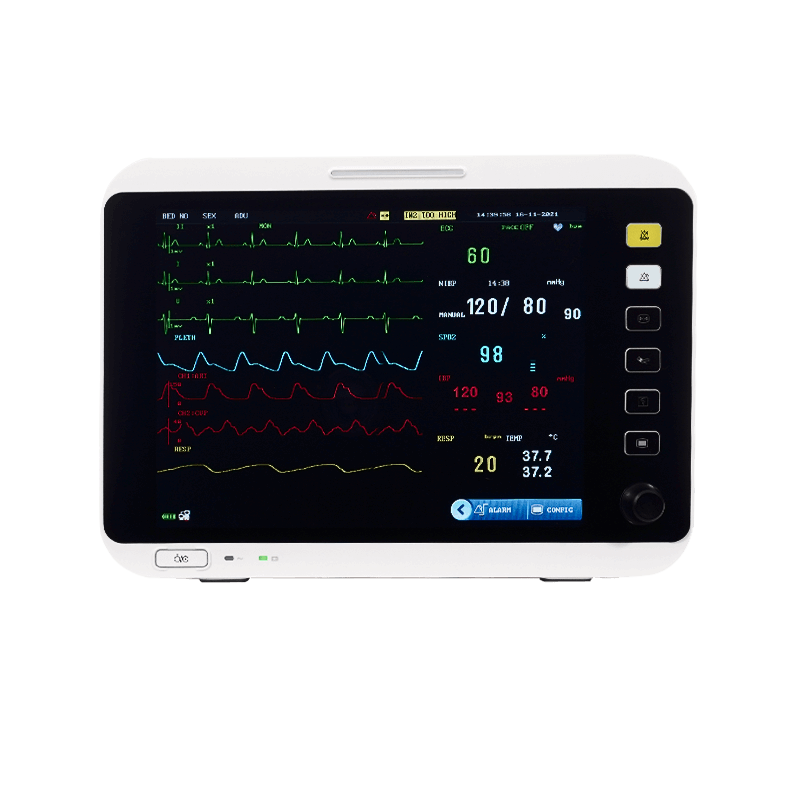
The patient monitor can detect some important vital signs parameters of patients in real time, continuously and for a long time, which has important clinical value. But also portable mobile, vehicle-mounted use, greatly improve the use frequency. At present, multiparameter patient monitor is relatively common, and its main functions include ECG, blood pressure, temperature, respiration, SpO2, ETCO2, IBP, cardiac output, etc.
1. Basic structure of the monitor
A monitor is usually composed of a physical module containing various sensors and a built-in computer system. All kinds of physiological signals are converted into electrical signals by sensors, and then sent to computer for display, storage and management after pre-amplification. Multifunctional parameter comprehensive monitor can monitor ecg, respiration, temperature, blood pressure, SpO2 and other parameters at the same time.
Modular patient monitor are generally used in intensive care. They are composed of discrete detachable physiological parameter modules and monitor hosts, and can be composed of different modules according to requirements to meet special requirements.
2. The usage and working principle of multiparameter monitor
(1) Respiratory care
Most respiratory measurements in the multiparameter patient monitor adopt chest impedance method. The chest movement of the human body in the process of breathing causes the change of body resistance, which is 0.1 ω ~ 3 ω, known as respiratory impedance.
A monitor typically picks up signals of changes in respiratory impedance at the same electrode by injecting a safe current of 0.5 to 5mA at a sinusoidal carrier frequency of 10 to 100kHz through two electrodes of the ECG lead. The dynamic waveform of respiration can be described by the variation of respiratory impedance, and the parameters of respiration rate can be extracted.
Thoracic movement and non-respiratory movement of the body will cause changes in body resistance. When the frequency of such changes is the same as the frequency band of the respiratory channel amplifier, it is difficult for the monitor to determine which is the normal respiratory signal and which is the motion interference signal. As a result, respiratory rate measurements may be inaccurate when the patient has severe and continuous physical movements.
(2) Invasive blood pressure (IBP) monitoring
In some severe operations, the real-time monitoring of blood pressure has very important clinical value, so it is necessary to adopt invasive blood pressure monitoring technology to achieve it. The principle is: first, the catheter is implanted into the blood vessels of the measured site through puncture. The external port of the catheter is directly connected with the pressure sensor, and normal saline is injected into the catheter.
Due to the pressure transfer function of the fluid, the intravascular pressure will be transmitted to the external pressure sensor through the fluid in the catheter. Thus, the dynamic waveform of pressure changes in blood vessels can be obtained. Systolic pressure, diastolic pressure and mean pressure can be obtained by specific calculation methods.
Attention should be paid to invasive blood pressure measurement: at the beginning of monitoring, the instrument should be adjusted to zero at first; During the monitoring process, the pressure sensor should always be kept at the same level as the heart. To prevent clotting of the catheter, the catheter should be flushed with continuous injections of heparin saline, which may move or exit due to movement. Therefore, the catheter should be firmly fixed and inspected carefully, and adjustments should be made if necessary.
(3) Temperature monitoring
Thermistor with negative temperature coefficient is generally used as temperature sensor in temperature measurement of monitor. General monitors provide one body temperature, and high-end instruments provide dual body temperatures. Body temperature probe types are also divided into body surface probe and body cavity probe, respectively used to monitor body surface and cavity temperature.
When measuring, the operator can put the temperature probe in any part of the patient's body according to need. Because different parts of the human body have different temperatures, the temperature measured by the monitor is the temperature value of the part of the patient's body to put the probe, which may be different from the temperature value of the mouth or armpit.
When taking a temperature measurement, there is a thermal balance problem between the measured part of the patient's body and the sensor in the probe, that is, when the probe is first placed, because the sensor has not yet fully balanced with the temperature of the human body. Therefore, the temperature displayed at this time is not the real temperature of the ministry, and it must be reached after a period of time to reach the thermal equilibrium before the actual temperature can be truly reflected. Also take care to maintain reliable contact between the sensor and the surface of the body. If there is a gap between the sensor and the skin, the measurement value may be low.
(4) ECG monitoring
The electrochemical activity of "excitable cells" in the myocardium causes the myocardium to be electrically excited. Causes the heart to contract mechanically. The closed and action current generated by this excitatory process of the heart flows through the body volume conductor and spreads to various parts of the body, resulting in a change in the current difference between different surface parts of the human body.
Electrocardiogram ( ECG ) is to record the potential difference of the body surface in real time, and the concept of lead refers to the waveform pattern of the potential difference between two or more body surface parts of the human body with the change of the cardiac cycle. The earliest defined Ⅰ, Ⅱ, Ⅲ leads are clinically called bipolar standard limb leads.
Later, the pressurized unipolar limb leads were defined, aVR, aVL, aVF and electrodeless chest leads V1, V2, V3, V4, V5, V6, which are the standard ECG leads currently used in clinical practice. Because the heart is stereoscopic, a lead waveform represents the electrical activity on one projection surface of the heart. These 12 leads will reflect the electrical activity on different projection surfaces of the heart from 12 directions, and the lesions of different parts of the heart can be comprehensively diagnosed.

At present, the standard ECG machine used in clinical practice measures the ECG waveform, and its limb electrodes are placed at the wrist and ankle, while the electrodes in the ECG monitoring are equivalently placed in the patient's chest and abdomen area, although the placement is different, they are equivalent, and their definition is the same. Therefore, the ECG conduction in the monitor corresponds to the lead in the ECG machine, and they have the same polarity and waveform.
Monitors can generally monitor 3 or 6 leads, can simultaneously display the waveform of one or both of the leads and extract heart rate parameters through waveform analysis. Powerful monitors can monitor 12 leads, and can further analyze the waveform to extract ST segments and arrhythmia events.
At present, the ECG waveform of the monitoring, its subtle structure diagnosis ability is not very strong, because the purpose of monitoring is mainly to monitor the patient's heart rhythm for a long time and in real time. But the ECG machine examination results are measured in a short time under specific conditions. Therefore, the amplifier bandpass width of the two instruments is not the same. The bandwidth of the ECG machine is 0.05~80Hz, while the bandwidth of the monitor is generally 1~25Hz. The ECG signal is a relatively weak signal, which is easily affected by external interference, and some types of interference are extremely difficult to overcome such as:
(a) Motion interference. The patient's body movements will cause changes in the electrical signals in the heart. The amplitude and frequency of this movement, if within the ECG amplifier bandwidth, the instrument is difficult to overcome.
(b) Myoelectric interference. When the muscles under the ECG electrode are pasted, an EMG interference signal is generated, and the EMG signal interferes with the ECG signal, and the EMG interference signal has the same spectral bandwidth as the ECG signal, so it cannot be simply cleared with a filter.
(c) Interference of high-frequency electric knife. When high-frequency electrocution or electrocution is used during surgery, the amplitude of the electrical signal generated by the electrical energy added to the human body is much greater than that of the ECG signal, and the frequency component is very rich, so that the ECG amplifier reaches a saturated state, and the ECG waveform cannot be observed. Almost all current monitors are powerless against such interference. Therefore, the monitor anti-high frequency electric knife interference part only requires the monitor to return to normal state within 5s after the high frequency electric knife is withdrawn.
(d) Electrode contact interference. Any disturbance in the electrical signal path from the human body to the ECG amplifier will cause strong noise that may obscure the ECG signal, which is often caused by poor contact between the electrodes and the skin. The prevention of such interference is mainly overcome from the use of methods, the user should carefully check each parts every time, and the instrument should be reliably grounded, which is not only good for combating interference, but more importantly, protecting the safety of patients and operators.
5. Noninvasive blood pressure monitor
Blood pressure refers to the pressure of blood on the walls of blood vessels. In the process of each contraction and relaxation of the heart, the pressure of blood flow on the blood vessel wall also changes, and the pressure of arterial blood vessels and venous blood vessels is different, and the pressure of blood vessels in different parts is also different. Clinically, the pressure values of the corresponding systolic and diastolic periods in the arterial vessels at the same height as the upper arm of the human body are often used to characterize the blood pressure of the human body, which is called systolic blood pressure (or hypertension) and diastolic pressure (or low pressure), respectively.
The body's arterial blood pressure is a variable physiological parameter. It has a lot to do with people's psychological state, emotional state, and posture and position at the time of measurement, the heart rate increases, the diastolic blood pressure rises, the heart rate slows down, and the diastolic blood pressure decreases. As the amount of strokes in the heart increases, the systolic blood pressure is bound to increase. It can be said that the arterial blood pressure in each cardiac cycle will not be absolutely the same.
Vibration method is a new method of non-invasive arterial blood pressure measurement developed in the 70s, and its principle is to use the cuff to inflate to a certain pressure when the arterial blood vessels are completely compressed and block the arterial blood flow, and then with the reduction of the cuff pressure, the arterial blood vessels will show a change process from complete blocking → gradual opening → full opening.
In this process, since the pulse of the arterial vascular wall will produce gas oscillation waves in the gas in the cuff, this oscillation wave has a definite correspondence with the arterial systolic blood pressure, diastolic pressure and average pressure, and the systolic, mean and diastolic pressure of the measured site can be obtained by measuring, recording and analyzing the pressure vibration waves in the cuff during the deflation process.
The premise of the vibration method is to find the regular pulse of the arterial pressure. In the actual measurement process, due to the patient's movement or external interference affecting the pressure change in the cuff, the instrument will not be able to detect the regular arterial fluctuations, so it may lead to measurement failure.
At present, some monitors have adopted anti-interference measures, such as the use of ladder deflation method, by the software to automatically determine the interference and normal arterial pulsation waves, so as to have a certain degree of anti-interference ability. But if the interference is too severe or lasts too long, this anti-interference measure cannot do anything about it. Therefore, in the process of non-invasive blood pressure monitoring, it is necessary to try to ensure that there is a good test condition, but also pay attention to the choice of cuff size, placement and tightness of the bundle.
6. Arterial oxygen saturation ( SpO2 ) monitoring
Oxygen is an indispensable substance in life activities. Active oxygen molecules in the blood are transported to tissues throughout the body by binding to hemoglobin (Hb) to form oxygenated hemoglobin (HbO2). The parameter used to characterize the proportion of oxygenated hemoglobin in the blood is called oxygen saturation.
The measurement of noninvasive arterial oxygen saturation is based on the absorption characteristics of hemoglobin and oxygenated hemoglobin in the blood, by using two different wavelengths of red light (660nm) and infrared light (940nm) through the tissue and then converted into electrical signals by the photoelectric receiver, while also using other components in the tissue, such as: skin, bone, muscle, venous blood, etc. The absorption signal is constant, and only the absorption signal of HbO2 and Hb in the artery is cyclically changed with the pulse , which is obtained by processing the received signal.
It can be seen that this method can only measure the blood oxygen saturation in the arterial blood, and the necessary condition for measurement is the pulsating arterial blood flow. Clinically, the sensor is placed in tissue parts with arterial blood flow and tissue thickness that is not thick, such as fingers, toes, earlobes and other parts. However, if there is vigorous movement in the measured part, it will affect the extraction of this regular pulsation signal and cannot be measured.
When the patient's peripheral circulation is severely poor, it will lead to a decrease in arterial blood flow at the site to be measured, resulting in inaccurate measurement. When the body temperature of the measuring site of a patient with severe blood loss is low, if there is a strong light shining on the probe, it may make the operation of the photoelectric receiver device deviate from the normal range, resulting in inaccurate measurement. Therefore, strong light should be avoided when measuring.
7. Respiratory carbon dioxide (PetCO2) monitoring
Respiratory carbon dioxide is an important monitoring indicator for anesthesia patients and patients with respiratory metabolic system diseases. The measurement of CO2 mainly uses infrared absorption method; That is, different concentrations of CO2 absorb different degrees of specific infrared light. There are two types of CO2 monitoring: mainstream and sidestream.
The mainstream type places the gas sensor directly in the patient's breathing gas duct. The concentration conversion of CO2 in the breathing gas is directly carried out, and then the electrical signal is sent to the monitor for analysis and processing to obtain PetCO2 parameters. The side-flow optical sensor is placed in the monitor, and the patient's breathing gas sample is extracted in real time by the gas sampling tube and sent to the monitor for CO2 concentration analysis.
When conducting CO2 monitoring, we should pay attention to the following problems: Since the CO2 sensor is an optical sensor, in the process of use, it is necessary to pay attention to avoid serious pollution of the sensor such as patient secretions; Sidestream CO2 monitors are generally equipped with a gas-water separator to remove moisture from the breathing gas. Always check whether the gas-water separator is working effectively; Otherwise, the moisture in the gas will affect the accuracy of the measurement.
The measurement of various parameters has some defects that are difficult to overcome. Although these monitors have a high degree of intelligence, they cannot completely replace human beings at present, and operators are still needed to analyze, judge and deal with them correctly. The operation must be careful, and the measurement results must be judged correctly.
Post time: Jun-10-2022